What is Vulvodynia?
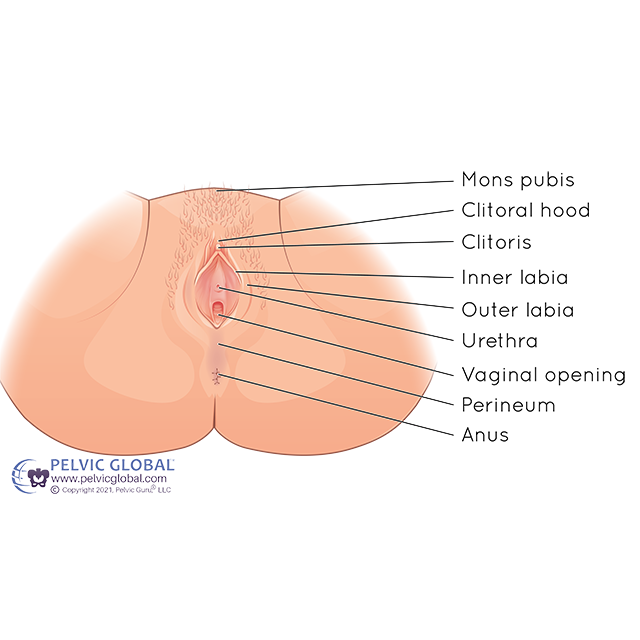
Permission to use copyright image from Pelvic Guru LLC
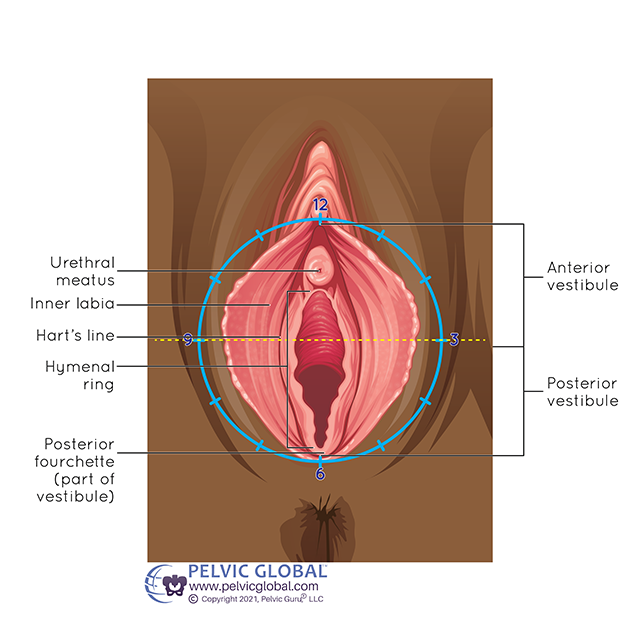
Vulvodynia is a general term for chronic vulvar pain (vulvo=vulva and dynia=pain). The vulva is the external genital tissue of someone assigned female at birth and includes the inner and outer labia, clitoris and vestibule (vaginal opening). It is thought to affect up to 16% of women(1), but unfortunately is often misdiagnosed and poorly understood. Vulvodynia can have negative impacts on both physical and mental health, and limit one’s ability to engage in daily life, social activities, work, and relationships.
Types
Localized: Pain is isolated to one area of the vulva.
Vestibulodynia: Pain is isolated to the vestibule (opening of the vagina).
General: Pain is experienced throughout the vulva sometimes varying at times or with different activities.
Provoked: Pain with touch to the vulva- sitting, donning
certain clothing, sexual activity, pelvic exams
Unprovoked: Pain is more constant, and without any of the above triggers.
Primary/Congenital: Pain has been present since the first attempt at inserting a tampon, sexual debut, and/or pelvic exam. There is a genetic component to the development of vulvodynia.
Secondary/Acquired: Pain starts after a period of pain-free tampon use, sexual intercourse, and/or pelvic exam. Vulvodynia is triggered after an injury, painful event, or infection.
Neuroproliferative: Nerves in the vulvar region become hypersensitive to input creating pain sensations.
Hormonally-Mediated: Hormonal changes like during menopause or with long-term oral contraceptive (birth control) use.
Inflammatory: Inflammation (due to chronic infections and/or environmental factors and irritants).
Permission to use copyright image from Pelvic Guru LLC
Symptoms
Symptoms include pain in the vulva. Pain may be itching, burning, stinging, sore, or aching in nature. There may be visible redness and swelling of the area. Vulvodynia can often be mistaken for a yeast infection so it is important to get tested for this prior to starting over the counter treatments. As mentioned above, pain may be provoked with sexual activity, tight clothing, or sitting for long periods of time, or may just occur randomly.
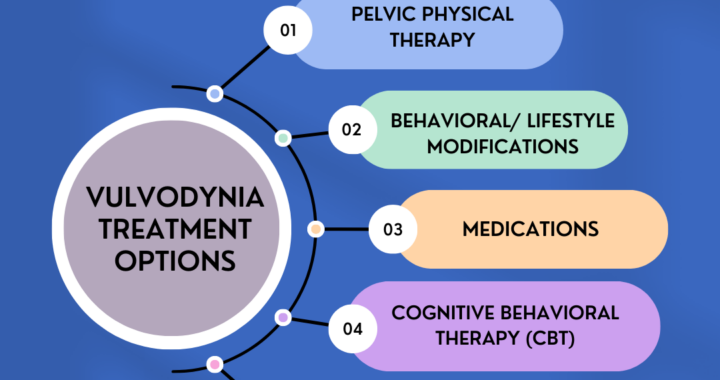
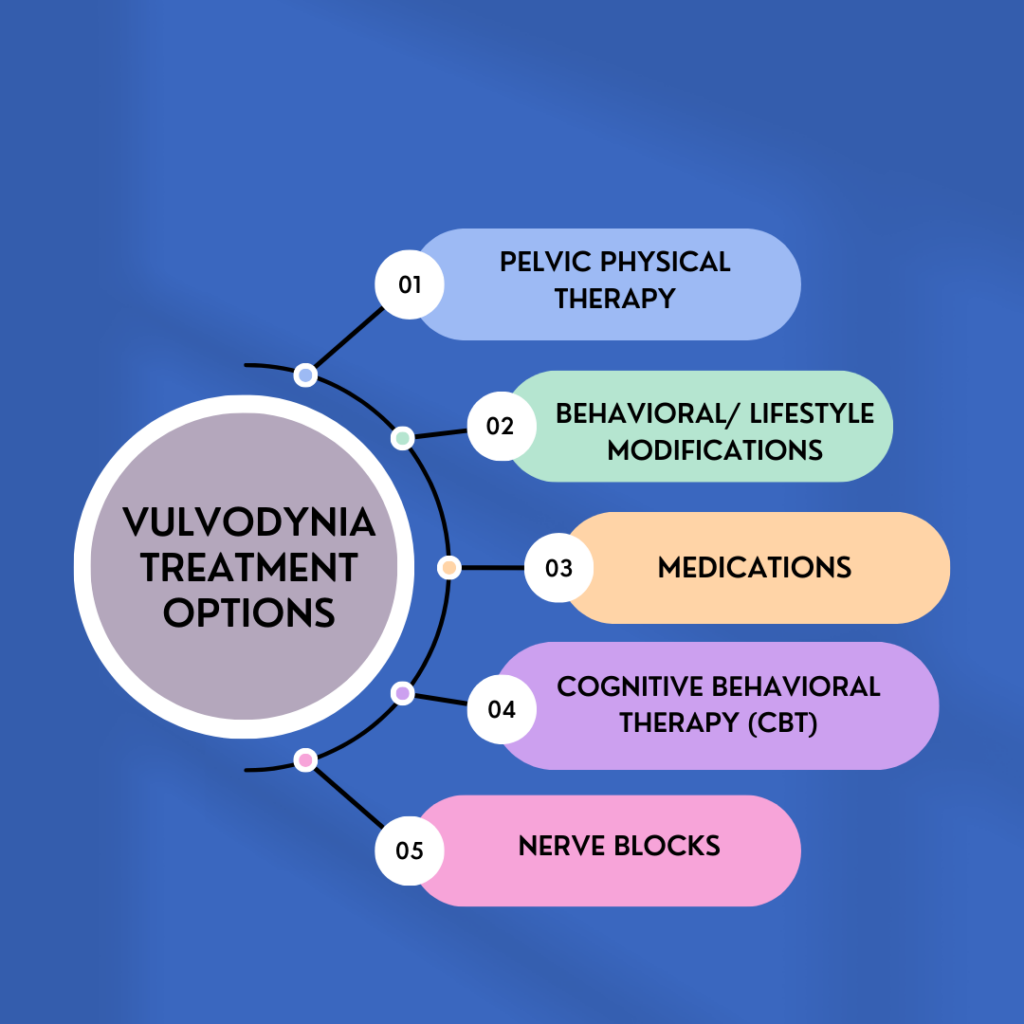
Treatment
Pelvic Floor Physical Therapy
Pelvic floor therapy with a physical therapist who has specialized training in pelvic health is a mainstay in treatment of vulvodynia. This may include manual therapy, exercises, and education to address muscle imbalances, pelvic floor muscle tension and tenderness, and improve overall function.
Behavioral/Lifestyle Modifications
This includes vulvar hygiene practices like washing the vulva with water only, patting the vulva dry, decreasing pad usage as able, and avoiding irritants in laundry detergent and soaps. It may also include other wellness practices like getting good sleep, eating a well balanced diet, and increasing general fitness and exercise
Medications
Topical and/or oral medications may be prescribed by your physician team. Depending on the underlying cause of your symptoms, these may include nerve medications (gabapentin, tricyclic antidepressants), steroid creams, and/or hormonal creams.
Cognitive Behavioral Therapy (CBT)
Because vulvodynia can have such an impact on many aspects of life, CBT can be helpful in managing the mental and emotional toll of this condition. It is usually helpful to find a practitioner who also has training in chronic pain management.
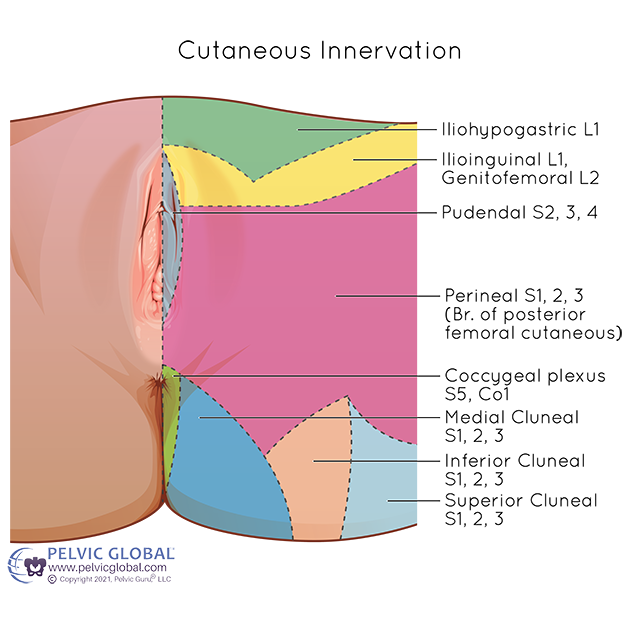
Permission to use copyright image from Pelvic Guru LLC
Nerve Blocks
If symptoms are thought to be driven by nerves, your physician team may recommend a local nerve injection. The pudendal nerve is most commonly treated, but depending on where your pain is (see image below), other nerves may be involved.
There is hope!
One study(3) showed that 83% of people did not seek additional treatment for vulvodynia after physical therapy because they experienced high levels of pain reduction afterwards- great news! So if you have been dealing with vulvodynia, give us a call today at (919)571-9912.
Resources
National Vulvodynia Association- www.nva.org
References
- Harlow BL, Stewart EG. A population-based assessment of chronic unexplained vulvar pain: have we underestimated the prevalence of vulvodynia? J Am Med Womens Assoc (1972). 2003 Spring;58(2):82-8. PMID: 12744420.
- Pukall, C.F., Mitchell, L.S. & Goldstein, A.T. Non-Medical, Medical, and Surgical Approaches for the Treatment of Provoked Vestibulodynia. Curr Sex Health Rep 8, 240–248 (2016). https://doi.org/10.1007/s11930-016-0093-y
- Jahshan-Doukhy O, Bornstein J. Long-Term Efficacy of Physical Therapy for Localized Provoked Vulvodynia. Int J Womens Health. 2021 Feb 10;13:161-168. doi: 10.2147/IJWH.S297389. PMID: 33603495; PMCID: PMC7882794.