Sitting on your last nerve?
Pelvic pain is a broad diagnosis. It can include any type of pain from the belly button to the sitting bones, front/ back/ saddle and groin region, lower abdomen, genitals. We get a lot of folks asking us about their symptoms and whether or not they have pudendal neuralgia (PN). Are you experiencing genital and or rectal pain that worsens with sitting? Do you have burning, aching pain in the vulva or perineum? If so, read on. If you suspect you may have PN, pelvic physical therapy can help.
Some of our patients have searched online to find out more about their symptoms, and it is not uncommon for them to come to us expressing fear that PN may be their diagnosis. The first step if you have PN is to learn more about what it is.
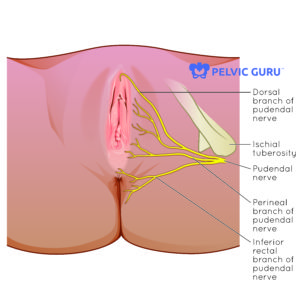
Permission to use copyright image from Pelvic Guru, LLC
Pudendal neuralgia means that there is pain along the path of the pudendal nerve, which innervates the pelvic region. The pudendal nerve (S2-4) is one potential contributor to pelvic pain. The pudendal nerve is peripheral nerve that courses through the pelvis from nerve roots at the sacrum and innervates the pelvic floor muscles, rectum, vagina and genitals. Innervation primarily comes from sacral nerve roots, with some contribution from the lumbar nerve roots L4-5. The pudendal nerve travels from the sacrum, near and through muscle and fascia, between the sacrotuberous and sacrospinous ligaments, in a sheath called Alcock’s canal and along the bony anatomy of the pelvis. It has a role in sensation and muscle contraction as well as a direct connection to the involuntary nervous system.
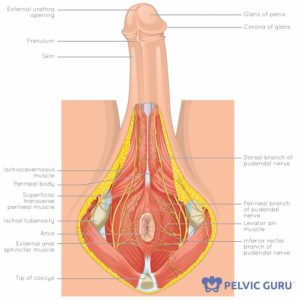
Permission to use copyright image from Pelvic Guru, LLC
When you have direct pressure on the nerve or it is placed on a prolonged stretch, the nerve may become sensitive. Direct pressure on the nerve may occur during or after prolonged sitting such long bike rides, travel, or repetitive sitting for prolonged periods of time. Chronic stretch of the nerve occurs with activities such as straining for bowel movements, heavy weight lifting or even childbirth. Muscle spasm or clenching of the pelvic floor muscles may also increase pressure on the pudendal nerve.
Diagnosis
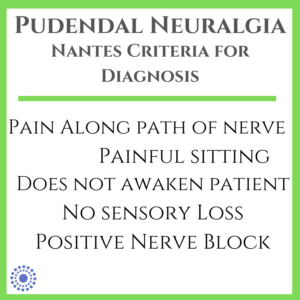
Spoiler alert: While exact prevalence is unknown, it is estimated that ~ 1/100,000 people (1, 2) or ~ 1% of the general population have PN. Not all genital pain, pelvic pain, painful sitting conditions are due to pudendal neuralgia. Specific diagnostic criteria, known as Nantes criteria (2,3) for diagnosing pudendal neuralgia include 5 components: Symptoms are along the distribution of the pudendal nerve, are worse with sitting, do not awaken the patient, does not include sensory loss upon exam, and is relieved by diagnostic nerve block.
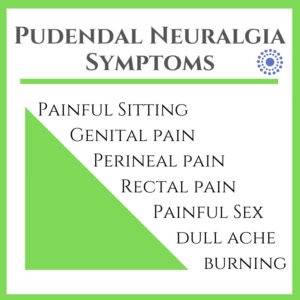
Other symptoms may also be factors in confirming a diagnosis of pudendal neuralgia. Common symptoms associated with irritation of the pudendal nerve include burning pain in the vulva, vagina, penis and/ or rectum, sexual dysfunction (pain and/or loss of erection and ability to orgasm) and bowel and/ or bladder urgency or pain. Your pelvic physical therapist likely has medical resources in the community for diagnostic procedures and testing.
You have pudendal neuralgia. Now what?
Our patients often come to us after spending some time on the interwebs and are really scared that they may have PN. First- knowledge is power and a sense of community is empowering! Finding information and others who have shared experiences is a wonderful thing. It can lead you to people who can help you learn more and how you can treat it. BUT. And this is a big but: If you have found yourself in a rabbit hole, chat room or information thread that leaves you scared, spinning and anxious, take some time away. Find a provider who can give you the facts about pudendal neuralgia and pain, answer your questions and point you to some of our PT colleagues for resources like this one at Pelvic Health & Rehabilitation Center and this one for all sorts of content and other references at Entropy Physio. Finding good information can help you focus on what is happening, who may be a helpful guide to your care and, most importantly, some paths to how you can start to feel better.
Treatment: Pelvic PT
 Physical therapy can be an effective first line of treatment to identify the various contributors to your symptoms and provide individualized care in order to return you back to your previous function as quickly as possible. Due to its path in the pelvis, a look at your mobility and how you move may help determine whether there is a mechanical factor in your symptoms. If you are experiencing these symptoms, a pelvic physical therapist can help you find ways to manage in the short term and improve your symptoms in the long term. Our therapists have specialized training in evaluating and treating those with pudendal neuralgia and other types of pelvic pain. We can also help you find other providers to ensure that your care is multi-disciplinary and specific to your needs. If you are experiencing any of the symptoms above and are ready to get started, give us a call at (919)-571-9912. We can’t wait to see you!
Physical therapy can be an effective first line of treatment to identify the various contributors to your symptoms and provide individualized care in order to return you back to your previous function as quickly as possible. Due to its path in the pelvis, a look at your mobility and how you move may help determine whether there is a mechanical factor in your symptoms. If you are experiencing these symptoms, a pelvic physical therapist can help you find ways to manage in the short term and improve your symptoms in the long term. Our therapists have specialized training in evaluating and treating those with pudendal neuralgia and other types of pelvic pain. We can also help you find other providers to ensure that your care is multi-disciplinary and specific to your needs. If you are experiencing any of the symptoms above and are ready to get started, give us a call at (919)-571-9912. We can’t wait to see you!
-
Hibner M1, Desai N, Robertson LJ, Nour M.J Minim Invasive Gynecol. 2010 Mar-Apr;17(2):148-53. doi: 10.1016/j.jmig.2009.11.003. Epub 2010 Jan 12.
-
Hibner, M, Castellanos, M, et al, Glob. libr. women’s med. (ISSN: 1756-2228) 2011; DOI 10.3843/GLOWM.10468
-
Labat JJ1, Riant T, Robert R, Amarenco G, Lefaucheur JP, Rigaud J. Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourol Urodyn. 2008;27(4):306-10.