The penis is a pretty amazing part of the body. It has some important jobs: an out-post for urine (check), a delivery system for semen and potential future children (check-check), and a pleasure center for partner and solo intimacy (check, check, check!). Keeping the penis in healthy working condition is a high priority for lots of those who have them- but what happens when your penis starts to hurt?
The penis is a pretty amazing part of the body. It has some important jobs: an out-post for urine (check), a delivery system for semen and potential future children (check-check), and a pleasure center for partner and solo intimacy (check, check, check!). Keeping the penis in healthy working condition is a high priority for lots of those who have them- but what happens when your penis starts to hurt?
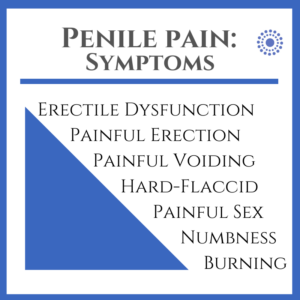
Symptoms
Yikes. These are the issues that bring many of our patients to our practice. Genital pain is no fun, especially in a body part that can be connected to pleasure AND is part of everyday bathroom function. Penile pain symptoms may include burning, numbness in tip, shaft or base; hard-flaccid symptoms and erectile dysfunction; painful voiding (urethra or deeper in the pelvis), painful arousal, erection, painful ejaculation or post-ejaculation pain; painful touch (ie during foreplay and/ or penetrative intercourse or sexual stimulation). Penile symptoms may be in isolation or accompanied by perineum, scrotum, testicle, rectal as well as back and hip pain. Symptoms may be associated with a specific trigger, out of the blue and intermittent or constant. Commonly reported triggers include sitting, exercise, arousal or sexual activity, bowel or bladder emptying and constipation. Stress, depression and anxiety may also be factors- either as a contributing mechanism or as an effect of living with genital pain.

When to see your doctor
Traumatic injury: Yes, it can happen! And if it happens to you for any reason- car accident, sports-related, sexual activity- it can cause damage to the soft tissue, nerve and blood supply of the penis and needs to be evaluated immediately.
Sudden or significant changes: Sudden change in genital sensation or in bowel/ bladder function requires immediate medical attention.
Change in appearance: Changes in your penis appearance- redness, warmth, discharge and/or other skin changes may be indicators of infection. Swelling, discoloration/ bruising and lack of retraction of the foreskin in those who are not circumcised require immediate medical attention. Sometimes people are embarrassed that they have pain in their privates- however, it’s important to see your primary care physician or urologist if you have any of the above symptoms. The penis’s visibility is one of its best features, so if you have one and don’t inspect it on the regular, there’s no time like the present.
If you go to the doctor and (great news!) you don’t have a sexually transmitted infection, cancer, or other condition that requires treatment OR, as is often the case, you have had some treatment but little or no change in your symptoms, fear not! There may be a musculoskeletal cause of your pain and treatment options that can help.
Musculoskeletal Factors
Muscles, ligaments and other soft tissue
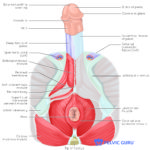
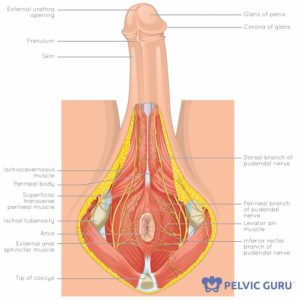
Permission to use copyright image from Pelvic Guru, LLC
Penis function relies on a healthy muscle system in order for optimal operations- erection, ejaculation, voiding. The urogenital muscles, in particular the bulbocavernosus and ischiocavernosus muscles have an important role in each of these tasks. Overactivity and/ or weakness of these muscles can result in muscle spasm and compression on nerves which may result in pain at the base, shaft or tip of the penis. Likewise, it may become painful or difficult to empty the bladder. Muscle tension or spasm of the deeper levator ani muscles may also refer pain to the penis or compress the pudendal nerve.
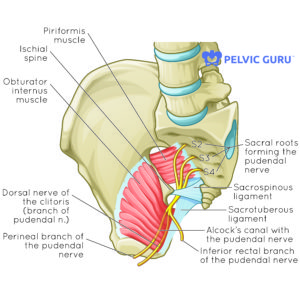
Permission to use copyright image from Pelvic Guru, LLC
Ligaments and other connective tissue as a whole provide support via their connections to our bony skeleton, muscles, organs and blood vessels. The pudendal nerve weaves a path from the sacrum, near and through muscle and fascia, between the sacrotuberous and sacrospinous ligaments, and in a sheath called Alcock’s canal and along the bony anatomy of the pelvis and is very connected to our hard and soft anatomical structures. There is variation in anatomy and in what is ‘normal’ movement from person to person, and most folks do just fine with their day to day activities without penis and genital pain. For those experiencing pain, spine and hip mechanics, breathing and general movement patterns should be assessed for possible compression and/ or stretch of the pudendal nerve and its surrounding structures.
Nervous System
Permission to use copyright image from Pelvic Guru, LLC
Both the central and peripheral nervous systems are considered when assessing penile pain. Peripheral nerves may be a factor in penile and genital pain, and the location may indicate which nerves may be involved. The ilioinguinal nerve (L1) / iliohypogastric (L1) has some distribution to the root of the penis. The dorsal nerve of the penis, a branch of the pudendal nerve (S2-4) is one of the primary suspects for shaft and glans pain. The pudendal nerve primarily comes from sacral nerve roots, with some contribution from the lumbar nerve roots as well. Due to its path in the pelvis from the sacrum, through the pelvis and to the penis, perineum, and anus, a look at your mobility and how you move may help determine whether there is a mechanical factor in your symptoms.
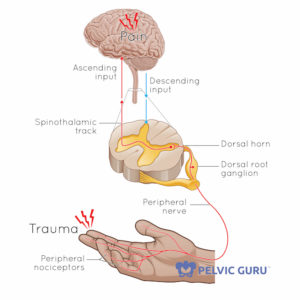
Permission to use copyright image from Pelvic Guru, LLC
The central nervous system (CNS) is the supercomputer that gives, receives and interprets all sorts of sensory and other data our we experience throughout the day. As much as we want to find ‘the reason’ we hurt, after we have pain for more than a few months our brain switches to ‘protection’ mode. This can sometimes lead to previously pain-free or pleasurable activities- sex, arousal, post-ejaculation- becoming off limits due to pain or fear of triggering a flareup. That said, we know that sometimes the discussion about the brain’s role in pain can feel a bit like ‘it’s all in your head.’ This couldn’t be further from the truth! It’s important that you feel you can trust your provider and that they listen and believe your pain history. It can take time to find the right team to treat you as a whole person. There are some excellent books, videos and other resources that do an excellent job of explaining the important role of the brain and CNS in pain, and why we need to include it in our treatment plan.
Treatment- Pelvic PT
 A skilled pelvic PT can help you identify the factors in your penile pain as well as a treatment plan to help you feel better. This may also include working with you regarding referral to other providers, including physicians, talk therapists and/ or sex therapists and other professionals to address all of your needs- it truly does take a village. Due to all of the mechanical, peripheral and central components that may factor into penile pain, treatment must be both from the top-down AND the bottom-up by:
A skilled pelvic PT can help you identify the factors in your penile pain as well as a treatment plan to help you feel better. This may also include working with you regarding referral to other providers, including physicians, talk therapists and/ or sex therapists and other professionals to address all of your needs- it truly does take a village. Due to all of the mechanical, peripheral and central components that may factor into penile pain, treatment must be both from the top-down AND the bottom-up by:
1)Quieting the CNS to reduce fear, avoidance, fight/ flight responses and
2) Optimizing movement and mechanics to reduce sensitivity, adverse tension and/ or compression on peripheral nerves.
Sessions are tailored to each person’s needs and often include a combination of education, hands-on techniques, relaxation strategies, yoga and various forms of exercise. Treatment always includes a home program to help you learn ways to feel better on your own.
We are adaptable to stresses placed on our bodies- this is how we learn new things, gain strength and coordination and recover from injury-this is a wonderful thing! So if some of this sounds like what you may be experiencing, remember that this adaptability of our soft tissues and nervous system can help you improve your penis pain and return to sex and other activities comfortably.
Next steps
If you have penis pain and want to know more about whether pelvic PT might help you, call us today at (919) 571-9912. We offer a complimentary 15 minute phone consultation to help determine if our physical therapists are the right fit for you!