This post is a personal one. I have some dear friends who have lost their parents to colorectal cancer. A friend recently shared that she has two colleagues with advanced colorectal cancer, both diagnosed in their 40’s. And a former patient inspired this post when she asked the question: “Why didn’t anyone talk to me about how this would affect my sex life?” Pelvic symptoms, including sexual dysfunction affect many people due to effects of both the cancer and the treatment. Pelvic PT can help if you or someone you know is living with the ongoing effects of colorectal cancer and management.
Colorectal Cancer Basics
- Prevalence: 2nd leading cause of cancer-related deaths in US (1,2)
- 4th most common cancer (2)
- Age: More than 90% of CR cancer is in those > 50 (1) BUT incidence of colorectal cancer diagnosis in those <50 is increasing, with ~ 75% of those diagnosed in their 40’s.(3)
Treatment & Side Effects
 The treatment for colorectal cancers is variable depending on type, location and severity. As with other forms of cancer and cancer treatment, side effects may occur during and after treatment- on a temporary long or short term basis or permanently.
The treatment for colorectal cancers is variable depending on type, location and severity. As with other forms of cancer and cancer treatment, side effects may occur during and after treatment- on a temporary long or short term basis or permanently.
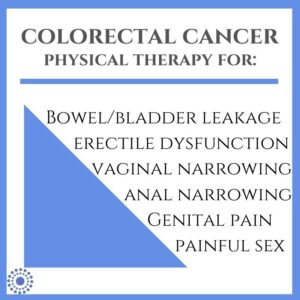
- Surgery- Surgery for colorectal cancers varies based on the type and stage of cancer, as well as location and tumor size. Short term side effects may be pain and activity changes related to surgical healing, as well as changes in bowel function such as in the case of colonostomy. Lower anterior resection surgery (LARS) has the highest incidence of adverse sexual effects.
- Radiation- Side effects of radiation during treatment include irritation to the rectal tissues, fatigue, bowel changes, and pain. Scarring of the tissues following radiation in the anus, rectum, and colon can cause changes in tissue pliability, muscular contractility, and sensation, which in turn may affect bowel, bladder and sexual function. Tissue changes due to radiation may continue to occur for several months following treatment. The vaginal canal may narrow (called vaginal stenosis) and limit penetrative intercourse. Erectile dysfunction and decreased sexual function can also occur. Radiation also can affect sperm as well as reduce sperm production, and can damage ovaries and trigger early menopause.
- Chemo- Many side effects of chemotherapy are localized to the time near treatment. However, due to systemic effects of certain types of chemotherapy, some may have long-term symptoms as a result of treatment. Neuropathy can affect sensation in the hands and feet, as well as sensitivity of the esophagus (5). Numbness, tingling, pain and sensitivity in these regions can have an impact and take up to 2 years to resolve or may be persistent, depending on the duration of treatment (6). Another side-effect reported in 1 in 5 people after chemotherapy is brain fog, which includes changes in alertness and memory.
- Vulvar & vaginal changes: Early menopause can begin due to above treatment, leading to dryness, vaginal atrophy, decreased libido and arousal as well as painful penetration may be experienced due to vaginal stenosis (narrowing) due to radiation and changes in sensation.
- Penis-perineum changes: Erectile dysfunction, sensory changes, decreased libido may be experienced.
- Bowel/ Bladder changes: Bowel-related effects include anal stenosis (narrowing) and damage to the small intestine known as radiation enteritis and proctitis (4). Incontinence may occur due to radiation changes to nerves and muscle as well as surgical changes depending on size, location and severity of the tumor.
Let’s talk about SEX
It’s not often that we talk about sex and colorectal cancer in the same sentence. As with any cancer, sometimes sex isn’t as high on the list as other immediate priorities of treatment. But what happens once you are feeling well enough during the course of treatment to explore intimacy again? While colorectal cancer has been sometimes thought of as affecting older people, colorectal cancer is increasingly being diagnosed in people in their 40’s. AND, most importantly, intimacy and sex is enjoyed by people at all ages, and it’s important to discuss this as a part of cancer care.
- Sexual dysfunction is reported in all genders following treatment for colorectal cancers (7,8). however sexual issues are rarely addressed or treated. Higher reports of sexual dysfunction after surgery, highest following abdominal-perineal resection both in function as well as in fear of ostomy leakage for those with ostomy, and general bowel changes for those without (8). Sensation of vagina feeling ‘smaller or tighter’ has also been reported after surgery.
- Pelvic pain, vaginal dryness and decreased libido/ lubrication associated with early menopause are also factors related to chemotherapy and radiation treatment.
- Self image: Change in sexual function- such as arousal, erection and pain or change in sensation during intimacy- can all affect one’s comfort when pursuing sex. Those with surgical changes, such as a colonostomy pouch and changes in managing bowels can affect self esteem and comfort with pursuing intimacy with an existing or new partner. Changes in continence due to treatment may also inhibit confidence and self image related to resuming sex.
Pelvic physical therapy: We can help!
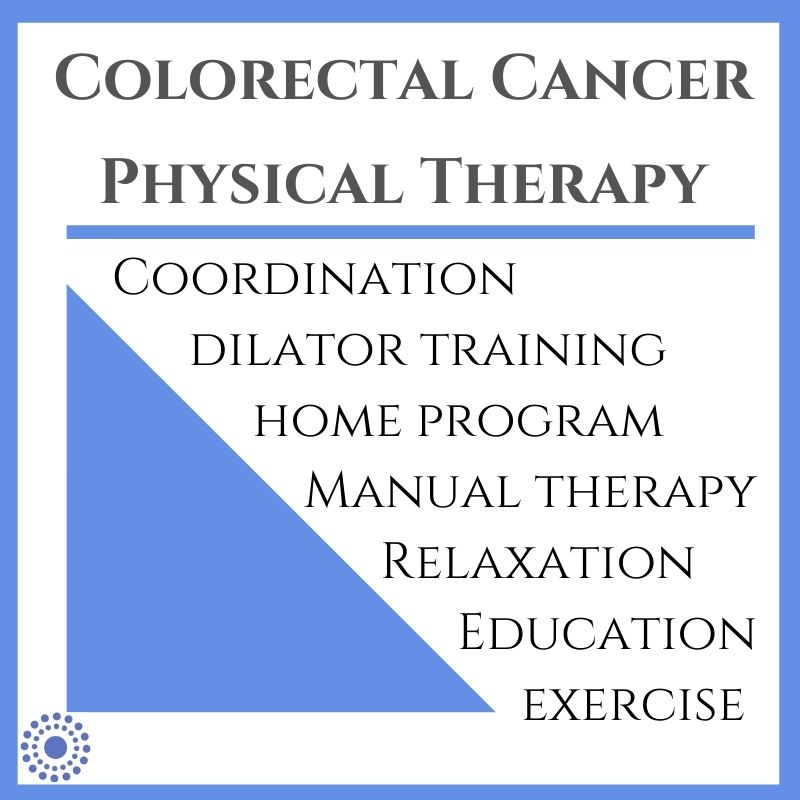
If you or someone you know is experiencing changes in bowel, bladder and/or sexual function, physical therapists can help to determine individualized plans to manage symptoms, address incontinence and improve soft tissue and muscular function to resume intimacy. Physical therapy sessions may include instruction in use of dilators and skin care to help keep tissues as healthy as possible. Coordination exercises for the pelvic and trunk muscles and general exercise and conditioning are part of a comprehensive program for all pelvic cancers and related treatment. Lastly, education about your body and setting goals that are important to you is an important part of your care. Your therapist will coordinate with your doctors as appropriate to guide your care based on your phase of treatment and recovery. We also work with talk therapists for those seeking additional strategies for coping with changes resulting from cancer care and treatment.
Call us today with questions about how physical therapy may help you at (919)-571-9912.
References:
- https://www.cdc.gov/cancer/dcpc/resources/features/colorectalawareness/
- https://healthfinder.gov/NHO/MarchToolkit.aspx
- http://fightcolorectalcancer.org/prevent/about-colorectal-cancer/facts-stats/
- Anal Cancer Foundation
- American Cancer Society- Chemotherapy For Colorectal Cancer
- Fight Colorectal Cancer
- Wafi Attaallah, Caglar Ertekin, Ilker Tinay, Cumhur Yege
- Hendren et al.